By Dr. Dineshani Hettiarachchi Sirisena
Although liver disease was once considered a disease of older men, this trend is changing. The face of liver cirrhosis has altered, with more and more young adults getting affected. This increase in rates has been attributed to an epidemic of fatty liver disease. Historically the main culprits were alcohol use and hepatitis C. However, with effective treatment for the latter cause, the focus is now on non-alcoholic fatty liver disease. To understand the reasons behind this alarming trend among young adults, we spoke to National Institute of Mental Health (NIMH) Acting Consultant Physician Dr. Sachith C. Wijesiriwardena (MBBS, MD).
[caption id="attachment_187576" align="alignright" width="209"] NIMH Acting Consultant Physician Dr. Sachith C. Wijesiriwardena (MBBS, MD)[/caption]
What are the emerging liver conditions in the young?
There are a few liver diseases that are found among the younger adult population, but currently the most prevalent is Non-Alcoholic Fatty Liver Disease (NAFLD). Historically it was the hepatitis C virus that was the most prevalent amongst the young, but due to increasingly effective treatment modalities and early detection, the prevalence has declined significantly. There are a few more rare conditions that can lead to cirrhosis, such as autoimmune hepatitis, Wilson’s Disease, and other genetic conditions.
What are the contributing/risk factors for NAFLD?
The main risk factors which contribute to NAFLD are as follows:
NIMH Acting Consultant Physician Dr. Sachith C. Wijesiriwardena (MBBS, MD)[/caption]
What are the emerging liver conditions in the young?
There are a few liver diseases that are found among the younger adult population, but currently the most prevalent is Non-Alcoholic Fatty Liver Disease (NAFLD). Historically it was the hepatitis C virus that was the most prevalent amongst the young, but due to increasingly effective treatment modalities and early detection, the prevalence has declined significantly. There are a few more rare conditions that can lead to cirrhosis, such as autoimmune hepatitis, Wilson’s Disease, and other genetic conditions.
What are the contributing/risk factors for NAFLD?
The main risk factors which contribute to NAFLD are as follows:
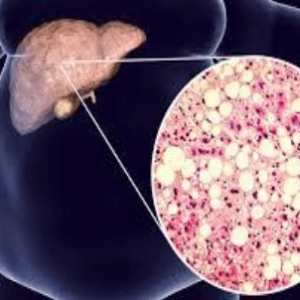 PHOTO © DRUGTARGETREVIEW[/caption]
Though not in high incidence, recent evidence shows that there is an increased likelihood for it to run in families. Genetic predisposition due to a single gene polymorphism linked to the short arm of chromosome 22 is associated with more severe NAFLD and in turn higher risk to progress to cirrhosis and hepato-cellular cancer. For people who have a family history of cirrhosis or liver cancer, it’s important to get screened early as it can be preventable if it occurs due to NAFLD.
How is it different from Alcoholic Liver Disease (ALD)?
Clinical history will indicate significant alcohol consumption which is usually more than 21 units per week. There usually is no significant family history in ALD.
Through an ultrasound scan, it is nearly indistinguishable, but histologically there are many features.
PHOTO © DRUGTARGETREVIEW[/caption]
Though not in high incidence, recent evidence shows that there is an increased likelihood for it to run in families. Genetic predisposition due to a single gene polymorphism linked to the short arm of chromosome 22 is associated with more severe NAFLD and in turn higher risk to progress to cirrhosis and hepato-cellular cancer. For people who have a family history of cirrhosis or liver cancer, it’s important to get screened early as it can be preventable if it occurs due to NAFLD.
How is it different from Alcoholic Liver Disease (ALD)?
Clinical history will indicate significant alcohol consumption which is usually more than 21 units per week. There usually is no significant family history in ALD.
Through an ultrasound scan, it is nearly indistinguishable, but histologically there are many features.
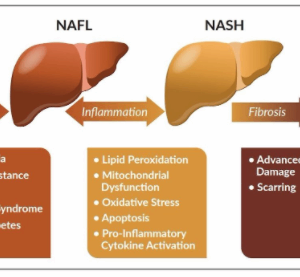 PHOTO © SANBIO[/caption]
Making a diagnosis
It’s predominantly a disease of exclusion. Conditions to be excluded include other causes of Chronic Liver Disease (CLD) such as viral hepatitis (B and C), plasma iron, iron binding capacity and ferritin levels (to rule out genetic disorders, which deposit iron in the liver), autoimmune conditions where antibodies produced by your body attack the liver (eg. ANA levels).
Classically when you undergo routine liver function tests the ALT and AST are above normal and ALT is slightly higher or equal to AST which points towards NAFLD (in ALD it is usually the AST which is higher than ALT at a ratio of 2:1). Then a routine ultrasound scan of the liver is performed, and a radiologist can easily detect fat deposition in the liver and grade it.
Serum ferritin levels are usually elevated in patients with NAFLD.
NAFLD is subdivided into Non-Alcoholic Fatty Liver (NAFL) where there is fat deposition but no inflammation and Non-Alcoholic Steato Hepatitis (NASH).
If there is suspicion of advanced fat deposition which causes inflammation of the liver – medically called NASH – the options are to go for a biopsy, or an advanced scan called the elastogram which is now available in certain hospitals. A biopsy is usually indicated if the clinician is not clear of the diagnosis or to assess the degree of liver injury and it is the only method available to differentiate NAFL from NASH.
Treatment options
The single most important step is weight loss. Mainly for the overweight (BMI >25 kg/m2) and obese (BMI >30 kg/m2) population, but thin people with central obesity are at risk as well. The primary target is to reduce 5-7% of body weight at the rate of 0.5-1.0 kg a week. This should be done by dietary modifications and exercise. The simplest way is to do a brisk walk of 30 to 45 minutes a day for four to five days a week.
Cutting down on carbohydrates is very important even if you don’t have Diabetes. Please see a nutritionist and get an appropriate dietary plan.
If you have Diabetes, strict control is necessary and if you have high cholesterol, then you need to control your condition with medications depending on the values and risk. Controlling blood pressure for patients with hypertension is paramount. These are termed risk factor modification and are an important step in treating NAFLD.
Vaccinations against hepatitis A and B need to be completed and you can speak to your general practitioner to evaluate your immunity status.
Ideally, abstain from alcohol or refrain from heavy drinking. It is also very important to note that if NASH is present the weight loss target is higher (7-10%), concluded Dr. Wijesiriwardena.
PHOTO © SANBIO[/caption]
Making a diagnosis
It’s predominantly a disease of exclusion. Conditions to be excluded include other causes of Chronic Liver Disease (CLD) such as viral hepatitis (B and C), plasma iron, iron binding capacity and ferritin levels (to rule out genetic disorders, which deposit iron in the liver), autoimmune conditions where antibodies produced by your body attack the liver (eg. ANA levels).
Classically when you undergo routine liver function tests the ALT and AST are above normal and ALT is slightly higher or equal to AST which points towards NAFLD (in ALD it is usually the AST which is higher than ALT at a ratio of 2:1). Then a routine ultrasound scan of the liver is performed, and a radiologist can easily detect fat deposition in the liver and grade it.
Serum ferritin levels are usually elevated in patients with NAFLD.
NAFLD is subdivided into Non-Alcoholic Fatty Liver (NAFL) where there is fat deposition but no inflammation and Non-Alcoholic Steato Hepatitis (NASH).
If there is suspicion of advanced fat deposition which causes inflammation of the liver – medically called NASH – the options are to go for a biopsy, or an advanced scan called the elastogram which is now available in certain hospitals. A biopsy is usually indicated if the clinician is not clear of the diagnosis or to assess the degree of liver injury and it is the only method available to differentiate NAFL from NASH.
Treatment options
The single most important step is weight loss. Mainly for the overweight (BMI >25 kg/m2) and obese (BMI >30 kg/m2) population, but thin people with central obesity are at risk as well. The primary target is to reduce 5-7% of body weight at the rate of 0.5-1.0 kg a week. This should be done by dietary modifications and exercise. The simplest way is to do a brisk walk of 30 to 45 minutes a day for four to five days a week.
Cutting down on carbohydrates is very important even if you don’t have Diabetes. Please see a nutritionist and get an appropriate dietary plan.
If you have Diabetes, strict control is necessary and if you have high cholesterol, then you need to control your condition with medications depending on the values and risk. Controlling blood pressure for patients with hypertension is paramount. These are termed risk factor modification and are an important step in treating NAFLD.
Vaccinations against hepatitis A and B need to be completed and you can speak to your general practitioner to evaluate your immunity status.
Ideally, abstain from alcohol or refrain from heavy drinking. It is also very important to note that if NASH is present the weight loss target is higher (7-10%), concluded Dr. Wijesiriwardena.
 NIMH Acting Consultant Physician Dr. Sachith C. Wijesiriwardena (MBBS, MD)[/caption]
What are the emerging liver conditions in the young?
There are a few liver diseases that are found among the younger adult population, but currently the most prevalent is Non-Alcoholic Fatty Liver Disease (NAFLD). Historically it was the hepatitis C virus that was the most prevalent amongst the young, but due to increasingly effective treatment modalities and early detection, the prevalence has declined significantly. There are a few more rare conditions that can lead to cirrhosis, such as autoimmune hepatitis, Wilson’s Disease, and other genetic conditions.
What are the contributing/risk factors for NAFLD?
The main risk factors which contribute to NAFLD are as follows:
NIMH Acting Consultant Physician Dr. Sachith C. Wijesiriwardena (MBBS, MD)[/caption]
What are the emerging liver conditions in the young?
There are a few liver diseases that are found among the younger adult population, but currently the most prevalent is Non-Alcoholic Fatty Liver Disease (NAFLD). Historically it was the hepatitis C virus that was the most prevalent amongst the young, but due to increasingly effective treatment modalities and early detection, the prevalence has declined significantly. There are a few more rare conditions that can lead to cirrhosis, such as autoimmune hepatitis, Wilson’s Disease, and other genetic conditions.
What are the contributing/risk factors for NAFLD?
The main risk factors which contribute to NAFLD are as follows:
- Central obesity
- Young hypertension (increased blood pressure)
- Dyslipidemia (blood cholesterol abnormalities)
- Diabetes mellitus or insulin resistance
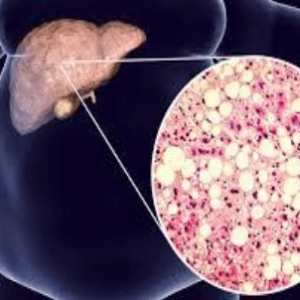 PHOTO © DRUGTARGETREVIEW[/caption]
Though not in high incidence, recent evidence shows that there is an increased likelihood for it to run in families. Genetic predisposition due to a single gene polymorphism linked to the short arm of chromosome 22 is associated with more severe NAFLD and in turn higher risk to progress to cirrhosis and hepato-cellular cancer. For people who have a family history of cirrhosis or liver cancer, it’s important to get screened early as it can be preventable if it occurs due to NAFLD.
How is it different from Alcoholic Liver Disease (ALD)?
Clinical history will indicate significant alcohol consumption which is usually more than 21 units per week. There usually is no significant family history in ALD.
Through an ultrasound scan, it is nearly indistinguishable, but histologically there are many features.
PHOTO © DRUGTARGETREVIEW[/caption]
Though not in high incidence, recent evidence shows that there is an increased likelihood for it to run in families. Genetic predisposition due to a single gene polymorphism linked to the short arm of chromosome 22 is associated with more severe NAFLD and in turn higher risk to progress to cirrhosis and hepato-cellular cancer. For people who have a family history of cirrhosis or liver cancer, it’s important to get screened early as it can be preventable if it occurs due to NAFLD.
How is it different from Alcoholic Liver Disease (ALD)?
Clinical history will indicate significant alcohol consumption which is usually more than 21 units per week. There usually is no significant family history in ALD.
Through an ultrasound scan, it is nearly indistinguishable, but histologically there are many features.
- Fatty degeneration of NAFLD in liver cells occurs to a greater degree than ALD
- Inflammatory cell infiltration is more pronounced in ALD
- Perivenular fibrosis (area surrounding vessels), phlebosclerosis (capillaries getting scarred), and less commonly lymphocytic phlebitis (white blood cells attacking the vessels) are more common in ALD
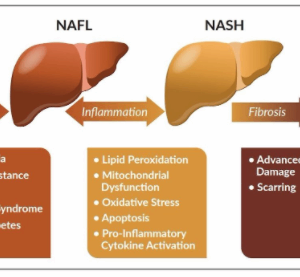 PHOTO © SANBIO[/caption]
Making a diagnosis
It’s predominantly a disease of exclusion. Conditions to be excluded include other causes of Chronic Liver Disease (CLD) such as viral hepatitis (B and C), plasma iron, iron binding capacity and ferritin levels (to rule out genetic disorders, which deposit iron in the liver), autoimmune conditions where antibodies produced by your body attack the liver (eg. ANA levels).
Classically when you undergo routine liver function tests the ALT and AST are above normal and ALT is slightly higher or equal to AST which points towards NAFLD (in ALD it is usually the AST which is higher than ALT at a ratio of 2:1). Then a routine ultrasound scan of the liver is performed, and a radiologist can easily detect fat deposition in the liver and grade it.
Serum ferritin levels are usually elevated in patients with NAFLD.
NAFLD is subdivided into Non-Alcoholic Fatty Liver (NAFL) where there is fat deposition but no inflammation and Non-Alcoholic Steato Hepatitis (NASH).
If there is suspicion of advanced fat deposition which causes inflammation of the liver – medically called NASH – the options are to go for a biopsy, or an advanced scan called the elastogram which is now available in certain hospitals. A biopsy is usually indicated if the clinician is not clear of the diagnosis or to assess the degree of liver injury and it is the only method available to differentiate NAFL from NASH.
Treatment options
The single most important step is weight loss. Mainly for the overweight (BMI >25 kg/m2) and obese (BMI >30 kg/m2) population, but thin people with central obesity are at risk as well. The primary target is to reduce 5-7% of body weight at the rate of 0.5-1.0 kg a week. This should be done by dietary modifications and exercise. The simplest way is to do a brisk walk of 30 to 45 minutes a day for four to five days a week.
Cutting down on carbohydrates is very important even if you don’t have Diabetes. Please see a nutritionist and get an appropriate dietary plan.
If you have Diabetes, strict control is necessary and if you have high cholesterol, then you need to control your condition with medications depending on the values and risk. Controlling blood pressure for patients with hypertension is paramount. These are termed risk factor modification and are an important step in treating NAFLD.
Vaccinations against hepatitis A and B need to be completed and you can speak to your general practitioner to evaluate your immunity status.
Ideally, abstain from alcohol or refrain from heavy drinking. It is also very important to note that if NASH is present the weight loss target is higher (7-10%), concluded Dr. Wijesiriwardena.
PHOTO © SANBIO[/caption]
Making a diagnosis
It’s predominantly a disease of exclusion. Conditions to be excluded include other causes of Chronic Liver Disease (CLD) such as viral hepatitis (B and C), plasma iron, iron binding capacity and ferritin levels (to rule out genetic disorders, which deposit iron in the liver), autoimmune conditions where antibodies produced by your body attack the liver (eg. ANA levels).
Classically when you undergo routine liver function tests the ALT and AST are above normal and ALT is slightly higher or equal to AST which points towards NAFLD (in ALD it is usually the AST which is higher than ALT at a ratio of 2:1). Then a routine ultrasound scan of the liver is performed, and a radiologist can easily detect fat deposition in the liver and grade it.
Serum ferritin levels are usually elevated in patients with NAFLD.
NAFLD is subdivided into Non-Alcoholic Fatty Liver (NAFL) where there is fat deposition but no inflammation and Non-Alcoholic Steato Hepatitis (NASH).
If there is suspicion of advanced fat deposition which causes inflammation of the liver – medically called NASH – the options are to go for a biopsy, or an advanced scan called the elastogram which is now available in certain hospitals. A biopsy is usually indicated if the clinician is not clear of the diagnosis or to assess the degree of liver injury and it is the only method available to differentiate NAFL from NASH.
Treatment options
The single most important step is weight loss. Mainly for the overweight (BMI >25 kg/m2) and obese (BMI >30 kg/m2) population, but thin people with central obesity are at risk as well. The primary target is to reduce 5-7% of body weight at the rate of 0.5-1.0 kg a week. This should be done by dietary modifications and exercise. The simplest way is to do a brisk walk of 30 to 45 minutes a day for four to five days a week.
Cutting down on carbohydrates is very important even if you don’t have Diabetes. Please see a nutritionist and get an appropriate dietary plan.
If you have Diabetes, strict control is necessary and if you have high cholesterol, then you need to control your condition with medications depending on the values and risk. Controlling blood pressure for patients with hypertension is paramount. These are termed risk factor modification and are an important step in treating NAFLD.
Vaccinations against hepatitis A and B need to be completed and you can speak to your general practitioner to evaluate your immunity status.
Ideally, abstain from alcohol or refrain from heavy drinking. It is also very important to note that if NASH is present the weight loss target is higher (7-10%), concluded Dr. Wijesiriwardena.